Tonsils are soft tissue masses that sit on each side of the throat. They are a component of the lymphatic system, which defends the body against infection, particularly respiratory infection (via WebMD). Because the tonsils’ primary function is to prevent germs from entering the body through the mouth and nose, they can become infected.
According to the Cleveland Clinic, healthy tonsils vary in size, just as people do. In a healthy state, they are typically pink. Tonsils that swell and turn red are most likely infected. This condition is known medically as tonsillitis. Tonsillitis is a common infection, particularly among children and adolescents. It can be caused by various pathogens, the most common of which is viral, per the American Academy of Pediatrics. Furthermore, tonsils can swell even when there is no indication of infection. However, swelling is more common when an infection is present.
Based on a recent study, 2% of outpatient visits are for sore throat symptoms. Therefore, it is critical to understand the causes of tonsillitis, common symptoms, potential complications, and when to see your healthcare provider.
What causes tonsillitis?
Tonsillitis can be caused by various viruses, bacteria, and other microbes. This is not surprising, given that the tonsils trap germs as they enter the body. According to News Medical Life Sciences, most tonsillitis infections are viral-related. These viruses include the influenza virus, adenovirus, common cold virus, and viruses that cause hand, foot, and mouth disease and mononucleosis.
In addition, bacterial infections, like viral infections, can happen. The most common bacterial cause is group A streptococcal infection, also known as the dreaded strep throat (via the National Health Service). The onset of bacterial strep is usually sudden, painful, and accompanied by fever.
Furthermore, the Mayo Clinic suggests that the immune system may be to blame if it overreacts to microbes that it usually fights off. In this case, the body may develop inflamed tonsils, leading to tonsillitis. It is important to note that as people progress through puberty and into adulthood, the tonsil’s immune response weakens, which is why adults do not get tonsillitis as frequently as children.
Diagnosing tonsillitis

If you suspect tonsillitis and have a sore throat that worsens or is accompanied by other symptoms, consult your doctor. Your provider will inquire as to when your symptoms began, and a physical examination will be carried out. They will use a light to view the tonsils in your throat and look inside your ears. Because swollen neck lymph nodes can occur with tonsillitis, your doctor will check for them. Finally, they will listen to your lungs and heart to rule out any secondary problems (via Mayo Clinic).
Following the exam, your doctor will decide whether additional testing is necessary. According to a study published in the European Archives of Oto-Rhino-Laryngology, testing to determine the cause of a sore throat may include a rapid strep test that can be performed in the office and provides results in a few minutes. A long Q-tip swab is used to rub the surface of each tonsil for this test. If the rapid test results are positive, you have a bacterial infection known as strep throat. If the test is negative, they may send the swab for culture, or if they do not suspect a bacterial infection, you will be given home remedies to relieve the symptoms.
Additional testing to determine the cause of your symptoms may be ordered if you are very ill. These tests may include blood work or, more commonly, a complete blood count (CBC), as well as a mononucleosis test and other tests as determined by your doctor.
What does tonsillitis look and feel like?

Khosro/Shutterstock
Tonsillitis symptoms vary from person to person. There is no single set of symptoms that applies to everyone. However, you should be aware of the common and obvious (as well as the less apparent) symptoms.
Researchers examined tonsil size variations in a study published in Cureus and discovered that tonsil size varies from person to person. Thus, looking at tonsil size alone may not indicate tonsillitis. Conversely, tonsillitis may be present if your tonsils are enlarged and red, causing difficulty swallowing.
According to the Cleveland Clinic, a painful or irritated throat may be the first sign of tonsillitis. Furthermore, some symptoms, such as stomachaches and nausea or vomiting caused by certain tonsil infections, may lead you to believe you have a stomach bug. Younger children are more likely to have stomach issues associated with tonsillitis. Fever of more than 100.4 degrees Fahrenheit and swollen lymph nodes in the neck are also common symptoms. In addition, when you examine your tonsils, you may notice white patches or a slimy gray or yellow film covering them, indicating the presence of an infection.
If your fever or symptoms worsen over a few days, see your doctor for a proper diagnosis and treatment.
Pediatric tonsillitis

NDAB Creativity/Shutterstock
According to an article in Children’s Health, tonsillitis is common in young and school-aged children. Younger children attract germs. They can be like tiny germ magnets. It’s normal for them to touch everything and put strange objects in their mouths as they learn and develop. Furthermore, while at daycare or school, they are exposed to other children, who multiply the germ population. As obvious as it may seem, your child’s first few years of life are all about dealing with the crud your child shares with you and the rest of the family.
The leading cause of tonsillitis in children is a viral illness that results in tonsil irritation, redness, and swelling, in addition to cold symptoms such as runny nose and congestion that may also result in a cough. Additionally, children are more likely than adults to develop a peritonsillar abscess and strep throat.
An article in Raising Children mentions the importance of observing your child for loss of appetite, lack of fluid intake, and difficulty swallowing, as these symptoms should not be ignored. Children’s bodies are smaller than adults, so if the symptoms, as mentioned earlier, are present along with swollen tonsils, you should get in touch with a doctor for an evaluation.
What is the difference between acute, chronic, and recurrent tonsillitis?

Zay Win Htal/Shutterstock
Tonsillitis can be an acute infection with sudden symptoms, or a chronic (or recurring) problem that flares up several times a year. It is critical to understand all three conditions, because treatment will vary.
According to the American Academy of Otolaryngology-Head and Neck Surgery, acute tonsillitis suddenly occurs in people of all ages, with children most affected. Children under the age of two, on the other hand, are usually unaffected. Acute tonsillitis is common in the winter, when germs are more prevalent.
In contrast, recurrent tonsillitis is defined by at least seven episodes of infection within a year or more than three episodes per year for two years. Furthermore, if you continue to have infections for more than two years, the number of infections per year decreases, and you may be advised to have your tonsils removed (per Texas Children’s Hospital).
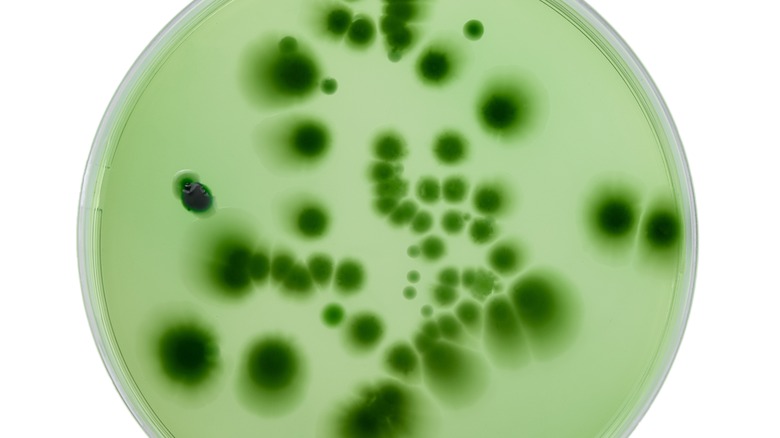
Similarly, chronic tonsillitis occurs frequently and may never go away completely. Science Direct mentions that tonsil pits may significantly cause chronic tonsillitis. These pits collect debris, creating an ideal environment for germs to hide and grow, leading to chronic infections. Your healthcare provider or an ENT specialist should examine you to determine whether you have a chronic condition that necessitates treatment or remedies to prevent infection recurrence.
What is a strep carrier?

Myboys.me/Shutterstock
A carrier of the group A Streptococcus bacterium is someone who has the bacteria in their throat or tonsils, but has no symptoms of illness caused by the bacteria. Upon examination, the throat and tonsils would be free of inflammation and redness, and no symptoms such as a sore throat or fever would be reported. The test would be positive if the throat were swabbed for strep throat, per Pediatrician Dr. Howard Bennett, MD.
The Centers for Disease Control and Prevention (CDC) noted that strep carriers are unlikely to spread the illness to others if they are not symptomatic. It is also important to note that if a carrier develops tonsillitis, it could be a viral form. They will, however, test positive for strep and will almost certainly be treated for strep throat if symptoms are present. It can be challenging to tell if the symptoms are caused by a virus or the step bacteria on someone that is a carrier.
Complications that can occur with tonsillitis

SrideeStudio/Shutterstock
Even though tonsillitis is a common infection that most people will encounter in their lifetime, it can lead to complications if left untreated. One complication that can occur is a peritonsillar abscess, also known as quinsy (via News Medical Life Sciences). An abscess can develop when an infection spreads in the tonsil and causes pus to form. When this happens, a specialist will likely need to drain the pus. Most people report quick relief after the abscess is drained.
Furthermore, as mentioned in an article in Stanford Medicine, your tonsils can grow more prominent with recurring infections, causing sleep disturbances, snoring, and possibly obstructive sleep apnea (OSA). OSA is common in children with very large tonsils. As a result of their muscles relaxing while sleeping, the tonsils can cause breathing obstruction. In this case, the tonsils may need to be surgically removed.
According to Nemours Kids Health, scarlet fever is another complication some kids get when their tonsillitis is caused by group A strep. Scarlet fever causes a bright red rash that typically starts on the neck and face and progresses to the rest of the body. It can appear like a bad sunburn. In this situation, it would be best if you have your child seen by a doctor, as antibiotics are needed to clear up this complication.
Tonsillitis and strep throat are two different illnesses

Pikul Noorod/Shutterstock
Tonsillitis is sometimes a catch-all term for a sore throat or strep throat. However, they are two distinct illnesses, per Healthline. Tonsillitis is caused by various germs, including viruses, fungi, bacteria, and allergens.
Healthline also mentions how tonsillitis and strep throat symptoms are similar, but strep throat may have some additional symptoms. In addition to fever and headache, both can cause sore lymph nodes in the neck, sore throat, and redness and swelling of the tonsils. In severe cases, strep throat may also cause nausea and vomiting, white pustules, body aches, and red spots on the tongue or mouth, as well as on the body.
Strep throat is caused by the group A Streptococcus bacteria, and will necessitate antibiotic treatment. If your child has cold-like symptoms such as a runny nose, cough, or red, itchy eyes, the cause of their sore throat is most likely viral, as strep throat does not cause these symptoms. Lastly, if a sore throat lasts more than a few days and worsens, you should see a doctor to determine the cause (via Healthy Children).
Do tonsil stones cause tonsillitis?

ShutterStockStudio/Shutterstock
Tonsil stones are not usually the cause of tonsillitis, but can form because of it. Tonsil stones are more likely to develop if you have frequent bouts of tonsillitis. Bacteria, mucus, and debris can accumulate as your tonsils fight infection. Usually, saliva washes away the debris that forms. However, any residue left behind can harden and turn into a stone (via WebMD).
According to CBHS Health, frequent tonsillitis episodes can lead to tonsil pitting. This pitting has the potential to trap food and gunk. It will calcify if it does not dislodge on its own. One of the main symptoms is bad breath, caused by calcified stones in the tonsils. Tonsil stones can develop without frequent bouts of tonsillitis, but tonsillitis can hasten the process. Furthermore, tonsil stones are more common in adults and may necessitate an adult tonsillectomy. Avoiding smoking, staying hydrated, and having good oral hygiene can prevent stone formation.
How is tonsillitis spread to others?

Da Antipina/Shutterstock
If you develop tonsillitis symptoms and are unsure of the cause, you should consider yourself contagious. Because most causes of tonsillitis are viral or bacterial infections, they can be passed on to others (per Healthline).
The CDC reports that respiratory droplets from one infected person to another are the most common mode of transmission of group A strep. These droplets are produced by talking, coughing, sneezing, and contact with saliva, nasal secretions, or shared cups or utensils. It is widespread in daycares and schools due to the large number of children close together and younger children who place everything they touch in their mouths. It’s recommended that a person infected with group A strep stay home until they are fever-free, and for a minimum of 12 hours after starting antibiotics.
Similarly, viral tonsillitis is spread the same way as bacterial or strep. Healthline also mentions that with the viral form, you could be contagious a day or two before developing symptoms, and should avoid close contact with others until symptoms improve.
When to see your healthcare provider for tonsillitis symptoms

Photoroyalty/Shutterstock
It is important to note that the COVID-19 pandemic caused concern for many people when they first developed sore throat symptoms. This is because sore throat was one of COVID-19’s common symptoms. Because of anxiety or fear of the virus, more people wanted to see their healthcare provider sooner rather than later (via Sharp Health News). But this begs the question: How do you know when you need to see a doctor?
Viruses cause most tonsillitis episodes. If you only have a sore throat and no difficulty swallowing, you may be able to treat your symptoms at home. According to MedicineNet, you should see your doctor if you have a high fever of more than 101 degrees Fahrenheit, difficulty swallowing or breathing, or visibly swollen tonsils.
Finally, if your symptoms do not improve after four days, consult your healthcare provider to ensure that there is no other cause.
Treatment for tonsillitis

Blackday/Shutterstock
Tonsillitis treatment will differ depending on the cause of the illness. Most viral infections are treatable at home with over-the-counter analgesics like acetaminophen or ibuprofen. Rest, plenty of fluids, and soft foods that won’t irritate the throat, such as yogurt, soup, bananas, or ice cream, are also advised, per WebMD.
In addition, MedlinePlus also suggests using a humidifier at night, avoiding cigarette smoke and secondhand smoke, and gargling with warm salt water (which can help alleviate symptoms). Throat lozenges are also a good option, as some include numbing ingredients that can provide relief.
Antibiotics will be prescribed if a bacterial infection, such as group A Streptococcus, is to blame. According to the CDC, penicillin or amoxicillin are the most prescribed antibiotics for strep throat. Cephalosporins can also be prescribed if you are allergic to penicillin medications. To ensure that the infection is cleared up, taking all the antibiotics as prescribed is critical.
When a tonsillectomy may be the best choice for a healthier life

Yuriy K/Shutterstock
Tonsillectomy is the surgical removal of the tonsils. This surgery is most commonly used to treat sleep-disordered breathing, but it is also used to treat recurrent or chronic tonsillitis when medical treatment is ineffective (via Mayo Clinic). Tonsillectomies are the most common procedure performed on children and teenagers, according to Nemours KidsHealth. However, medical professionals are beginning to perform fewer surgeries than in the past, because some research indicates that enlarged tonsils shrink as the child ages.
That said, tonsillectomies are required when the tonsils become so large that they block the airway and make breathing difficult. This frequently occurs during sleep as everything relaxes. If OSA is present, a tonsillectomy is required, because apnea episodes can lead to other health problems. Before performing surgery, your surgeon may request a sleep study to determine the severity of the breathing disorder.
If you or your child has trouble sleeping due to large tonsils or recurring infections, it is critical to discuss all your options to determine if a tonsillectomy is the best option for improved health.




